Healthy Births for Healthy Mothers and Babies
Becoming a parent is full of new, exciting and sometimes difficult experiences and decisions. You may already have an idea of the kind of pregnancy and birth experience you would like, or you may not even know where to start there’s so much to take in! For every mother, the most important outcome is a safe and healthy mother and baby, but as more women are discovering, a healthy birth can be a wonderful and empowering event at the same time.
AIMSI ‘s campaigns reflects a positive perspective of birth as a healthy, normal physiological event in a woman’s life and that of her baby. Healthy birth has long term affects on the health of women and babies. For this reason, birth practices, care, and treatments in pregnancy, labour, and birth should reflect the protection of the health of mothers and babies.
Health
/helTH/ Noun
1.The state of being free from illness or injury: “he was restored to health”; “a health risk”.
2.A person’s mental or physical condition.
For a long time, the quality of maternity care has been measured by the rate of deaths to mothers and babies. But, many now argue that this is not a true reflection of care as technology, nutrition, disease control, and hygiene have reduced the rate of deaths drastically. Instead, a way of measuring care is to look at the rates of complications that arise in pregnancy, and during labour, birth, and the postpartum period. These complications are called morbidity and can affect the health of mothers and babies ranging from moderate to severe harm. Some procedures and care increase the chances of these complications and, as a result, morbidity is on the rise in Ireland.
“Results have shown that maternal morbidities in Ireland are common and changing. Analysis of national trends in maternal morbidities from 2005-08 show a statistically significant increase in rates of postpartum haemorrhage (PPH), pelvic and perineal trauma, and gestational diabetes.Over an 11 year period (1999-2009), the overall PPH rate increased from 1.5% to 4.1%, with a significant increase in the rate of blood transfusion co-diagnosed with atonic PPH.”
“Further increasing rates of Caesarean section have led to an increase in the incidence of peripartum hysterectomy for morbidly adherent placenta. Such findings stress the need for continued surveillance of maternal morbidities to guide clinical practice, focusing on aetiological factors, preventative measures and quality of care.”
Measuring maternal morbidity, Edel Manning
AIMS Ireland are concerned about rising intervention rates, which can vary greatly between hospitals and even between individual health care providers. Interventions are known to increase the chances of harm to the physical and psychological health of mothers and babies. We all want mothers and babies to come through birth feeling healthy and emotionally complete.
Some procedures that are used in labour are shown to increase the chances of interventions which may cause harm to the health of mothers and babies. These procedures should be avoided but often are used routinely in Irish maternity units, which is not best practice. There are times when medical issues arise and intervention is required. Dr. Amali Lokugamage, an obsetrician in the UK, has spoken about the importance of maintaining aspects of normal birth during these occasions saying, “In case of emergencies and induction: rescue as many elements of physiological birth as possible” , and also, “let’s humanise high risk status”. We can be much kinder.
Some women request the use of procedures and intervention. As the main advocate in her pregnancy and birth, we must respect the desires and needs of mothers and provide her with all the information required – benefits, risks, alternatives – in order to make an informed decision for her and her baby.
In Ireland, we need to change our view of what is ‘normal’ in maternity care.
Ireland’s maternity services widely reflects an obstetric, hospital based maternity system. The majority of women are low-risk and will enjoy a healthy pregnancy and birth if supported by appropriate care. For most women, midwife led care is the recommended care option as evidence has shown this leads to less interventions. In Ireland, only a small number of women will have access to midwife-led care, at home or in hosital. The majority of our maternity care is based on an obstetric medical care model, which means consultant obstetricians lead the care and policies, not midwives.
Midwife-Led Care for a Healthy Pregnancy and Birth
The midwife is the expert in normal birth with extensive professional training and specialist skills. The World Health Organisation recognises the midwife as the most appropriate caregiver for women with healthy, normal pregnancies and births (WHO 1997). Obstetricians have special training in high-risk pregnancy and surgery and are therefore appropriate caregivers for women with established serious medicalconditions or who are at high risk for developing such conditions. The WHO says that at least 85% of pregnancies are low risk. With appropriate care, 70 to 80% of all pregnant women will have an uncomplicated labour.
What Is Midwife-Led Care?
The Royal College of Obstetricians and Gynaecologists defines midwife-led care as where “the midwife is the lead professional in the planning, organisation and delivery of care given to a woman from initial booking to the postnatal period” (RCOG, 2001). Currently in the Republic of Ireland midwife-led care is available at two midwife-led units (MLUs), in home birth with a self employed community midwife (SECM) and through some community midwifery schemes.
A review of relevant scientific research found that midwife-led care offers the greatest benefits to pregnant
women and their babies and recommends that this care be offered to most women. (Hatem et al., Midwife-led versus other models of care for childbearing women, Cochrane Database of Systematic Reviews, 2008) A recently published study of Ireland’s two MLUs at Cavan General Hospital and Our Lady of Lourdes Drogheda by Trinity College Dublin praises the midwife-led care practiced in these units, finding it as safe as consultant-led care and with lower intervention rates and higher satisfaction among women. Plus, the study found the MLUs to be more cost-effective. The authors recommend that MLUs be established throughout Ireland. (Report of the MidU Study, HSE, 2009)
Lower intervention rates are an important aspect of healthy birth. Many interventions have complications which unintentionally may lead to further interventions. For this reason, a labour is no longer considered ‘low risk’ once interventions begin, and one intervention often leads to a series of interventions.
Common Interventions include:
* induction of labour (starting your labour artificially)
* augmentation of labour (speeding up your labour)
* artificial rupture of the membranes (ARM)
* using medication for pain relief
* electronic fetal monitoring – external CTG or internal fetal scalp
* managed third stage of labour (delivering the placenta)
* coached pushing
* restricted birthing positions
* immediate cord clamping
* seperation of mother and baby in surgery/recovery
Common Complications include:
* post partum haemorrhage (PPH)
* perineal trauma
* episiotomy
* instrumental (assisted) delivery by forceps or ventouse
* admission to SCBU (special care baby unit) or NICU (neonatal intensive care unit)
* Caesarean section
* psychological morbidity – post traumatic stress disorder (PTSD), birth trauma
These interventions are the primary cause of maternal morbidity, but recent research has emerged to support the health effects (also called neonatal morbidity) of these interventions on an infant during labour, birth and postnatally. For example, an epidural and the use of drugs to induce/augment labour are often used together. Many women are not told about the effects these drugs can have, for example, on breastfeeding. Studies (5,6) are now showing that infants are slow to ‘suck’ when a mother is given these interventions, which can be extremely detrimental to the breastfeeding relationship. If this is the method of feeding a mother has chosen, she may be blaming herself for the supposed lack of ability to breastfeed, when it may have much more to do with the side effects of the drugs she was given in labour.
Another health effect of using medications to induce labour is that a first time mother will double her chances of a C-section compared to if she was allowed to go into spontaneous labour (7). This means that there is a domino effect as described above – often referred to as a ‘cascade of interventions’. If a mother is given one intervention, she will often find that another is needed, and then another – which increases the chances of an instrumental or C-section delivery. The effects of one or more interventions on an infant are too difficult to ascertain, particularly when they occur together, because it is hard to know which intervention is correlated with a baby who is experiencing neonatal morbidity. However, there is robust research that shows a correlation between the increase in neonatal respiratory morbidity and C-sections. What is most striking is that: while a baby born at 40 weeks has a 1.5% risk of neonatal respiratory morbidity, this jumps to 2.1% risk at 39 weeks, 5.1% at 38 weeks and 10% at 37 weeks (8). There are similar health risks to a baby when labour is induced pre-term (35 to 37 weeks). Even if a baby appears large and healthy at 36 weeks, it is still significantly less developed than a baby born when it is ready – sometime between 37 and 42 weeks.
Nature is not perfect. However, when it comes to babies and birth, unless there is a clear medical indication that induction of labor will do more good than harm, nature beats science hands down. For both mothers and babies, it is safe and wise to wait patiently until labor begins on its own. (9)
What all of the research above shows most starkly is that for the overall health of mothers and babies, a healthy birth involves learning and understanding the risks involved in interventions and making an informed choice or an informed refusal of the options given to you.
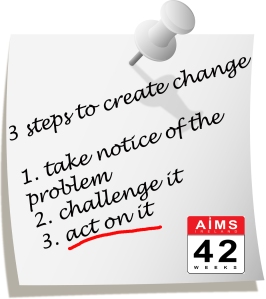
At 42 weeks, we want to change the way we look at birth in Ireland. Over the next 42 weeks we aim to review different topics which we feel will get women talking, highlight positive healthy birth in Ireland, and take notice of where and how we can be kinder, more evidence based, and healthier in the care we provide to mothers and babies. Be a part of it, help change the mindset of birth in order to provide healthy births for healthy mothers and babies! Share 42 weeks with your friends, contribute your own positive story or image, talk about healthy birth, choose healthy birth. Make healthy birth, normal birth in Ireland!
42 weeks define ‘healthy birth’ as:
* The mother is the advocate for her pregnancy and baby and should be the centre of the decison process.
* Pregnancy, Labour, Birth should be considered healthy unless there is a medical reason to suggest otherwise.
* Care should be individualised reflecting the needs, desires, history, and current needs of each mother and baby throughout pregnancy, labour, birth and postnatal periods.
* All care options are available to women based on individual assessment, rather than blanket criteria.
* Care should reflect the best evidence available, not individual practice, hospital policy, or medical instiutions.
* Mothers should have access to a wide range of care options regardless of region. These include midwife-led care, homebirth, and traditional consultant led care.
* Clear, unbiased, accurate, and readily available information in plain language – discussing benefits, harms, and alternatives – should be provided to women in order to assist with informed decision making.
* Mothers make the decisions which affect their health and the health of their baby: this includes to consent, to refuse, to ask for more time, to seek alternatives. Mothers’ decisons are final and are to be respected.
* Care is with considerate, respectful, and dignified.
* In case of emergencies and induction: rescue as many elements of physiological birth as possible.
(Dr. Lokugamage, Obstetrician, UK)
AIMS Ireland offers independent support and information on maternity choices and care to women and their families. We believe that every woman should have access to evidence-based maternity care that is appropriate to her individual needs, and that she should be enabled and empowered to be an active partner in that care.
References:
1.) Intro: AIMS Ireland Healthy Birth Directory for the West of Ireland: http://www.aimsireland.com
2.) Promoting, protecting, and supporting normal birth: a look at the evidence.http://www.ncbi.nlm.nih.gov/pubmed/18226163
3.) RCOG Making Normal Birth a reality: http://www.rcog.org.uk/womens-health/clinical-guidance/making-normal-birth-reality
4.) Measuring maternal morbidity, Edel Manning: http://www.ucc.ie/en/npec
5.) Newborn feeding behaviour depressed by intrapartum oxytocin: a pilot study, Fernandez et al. (July 2012), Acta Paediatrica, 101(7), pp. 749-754
6.) Labour epidural anasthesia, obstetric factors and breastfeeding cessation, Dozier et al. (June 2012), Maternal and Child Health Journal
7.) US Hospitals held accountable for C-section rates, Rebecca Dekker (January 2013) at www.evidencebasedbirth.com
8.) Hospitals are ignoring advice on c-sections, Denis Campbell (May 2, 2013), The Guardian http://www.guardian.co.uk/society/2013/may/02/early-caesarean-baby-health-risk
9.) Saying ‘No’ to Induction, Judith Lothian, (Spring 2006), Journal of Perinatal Education, 15(2), pp. 43-45
 AIMS Ireland
AIMS Ireland