The Mysterious Placenta and the Third Stage of Labour
Did you know, the placenta has always been thought of as a mysterious and powerful organ?
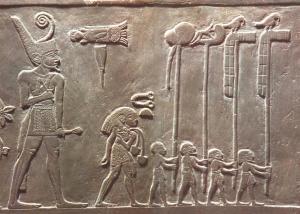
Since ancient times, the placenta has been a great source of mystery and importance. Many cultures have viewed the placenta as a ‘second self’ or an ‘external soul’. For example, Egyptian sculptures show a Pharaoh and attendants in a ceremonial procession carrying the Pharaoh’s ‘soul’ or ‘secret helper’ (the placenta with the umbilical cord) while Hebrew scriptures include several references to the placenta, referred to as the ‘bundle of life’ or the ‘external soul’. The Greeks knew that the placenta was integral to fetal nutrition and it is believed that Aristotle was one of the first philosopher-medics to use the term ‘chorion’ to describe the embryonic membranes that encompass the fetus. It is apparent that throughout history, the placenta was known to provide nourishment for the developing fetus, but it was not until the late 18th century to early 19th century that the mystery of the separate nature of maternal placental circulation to that of the fetus was discovered. (Longo, L. and Reynolds, L., 2010).
With the advent of ultrasound technology, there are now various ways of measuring the health of the placenta, thereby understanding the healthy development of the fetus. For example, using Doppler to measure blood flow or ultrasound to ascertain where the placenta is located.
When does the placenta start to grow?
At the time of implantation – around 6 to 12 days after conception – the networks of capillaries, cords and blood vessels begin to grow and merge together as a newly developing placenta. At this time – around 4 weeks after the last menstrual period (LMP) or 2 weeks after conception – the zygote that formed after fertilisation has travelled down the fallopian tube towards the uterus. This rapidly dividing ball of cells separates into two sections: the inner group of cells will become the embryo and the outer group of cells will burrow into the uterine wall for nourishment. The placenta begins to form at this time.
What does the placenta do?
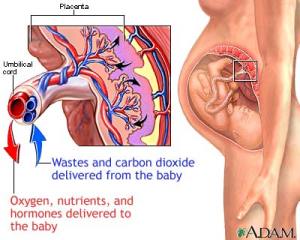
The main function of the placenta is to provide nutrition to the developing fetus. Blood from the mother goes through the placenta into the attached umbilical cord and into the blood of the growing fetus. This blood contains oxygen, glucose and other nutritional substances. The placenta acts a filter to ensure harmful substances are reduced and nutritional substances are passed on to the baby. In addition, the placenta acts like a ‘lung’ for the baby, allowing for the transfer of oxygen and for any waste products to be released into the mother’s circulation and to be disposed of in the mother’s urine.
Does the placenta move during pregnancy?
When the placenta first develops, it is often ‘low lying’ but will be carried up towards the top of the uterus as the pregnancy progresses. If the placenta does not move away from this low lying position closer to full term, it may be diagnosed as ‘placenta previa’, however, this occurs in less than 1% of pregnancies at term. Placenta previa can often be misdiagnosed – prior to 34 weeks – due to increased ultrasounds in the second trimester that show a low lying placenta before it has ‘migrated’ upwards. Placental migration is believed to be anywhere from 0.3mm/week (in women who have had a prior c-section delivery) up to 5.4mm/week in women who have had a previous vaginal delivery. The placenta moves at a different rate according to whether the placenta is in a posterior position (slower rate of migration), compared with an anterior position (faster rate of migration). The take home message is that it is extremely normal for the placenta to present as ‘low lying’ up to 34 weeks of pregnancy and that in over 99% of cases, the placenta will migrate upwards (and out of the way of the cervical opening) before a woman goes into labour.
How do placental hormones contribute to pregnancy, labour and birth?
The placenta releases hormones that are necessary for maintaining the optimum environment and nutrition for the developing fetus. The main hormones that are integral in the development of a growing baby – from conception to birth – are:
- Human Chorionic Gonadotrophin (hCG)
- Human Chorionic Somatomammotrophin (hCS)
- Oestregen
- Progesterone
From conception, these hormones are responsible for ‘setting the stage’ for all things pregnancy related, such as: optimum fetal development, preparing the pregnant woman’s body for lactation, signalling the onset of labour and expelling the placenta or ‘after-birth’.
Pregnancy is often associated with ‘morning sickness’, particularly in the first trimester when rapid changes in hormone levels occur and the placenta is developing. The first 12 weeks of pregnancy provide a foundation for the significantly accelerated growth that takes place once the placenta takes over hormonal and nutritional functioning.
Did you know that the human fetus increases its weight 6 billion times from conception to delivery?
What is the ‘third stage of labour’?
When it is time for labour to begin, the woman’s body will show signs that the baby is ready to be born. It is still a mystery as to what exactly occurs to initiate spontaneous labour with some theories saying it is due to the release of oxytocin in the pregnant woman while others say that it occurs when the fetus secretes a protein from its lungs. More than likely it is a combination of maternal and fetal signals that initiate the onset of labour. In a normal birth, various hormones work together during labour to facilitate uterine contractions and the movement of the baby down the birth canal.
After a woman has laboured (stage 1) and birthed her baby vaginally (stage 2), the hormones continue to signal to the placenta that it is safe to deliver the ‘after birth’ or placenta. This is known as the ‘third stage of labour’. Until recently, a Cochrane review on ‘Active versus expectant management in the third stage of labour’ suggested that administration of synthetic oxytocin (Syntocinon® or Syntometrine®) is preferred to expectant management – or simply allowing the placenta time to peel away from the uterine lining and to be expelled. This review has since been withdrawn.
A decision on whether to consent to the administration of uterotonic medications, or not, is very much related to each individual and the factors associated with their birth. If there are no signs of excessive blood loss, or postpartum haemorrhage (PPH), and a woman prefers to deliver the placenta without medication then it is her choice. Likewise, if a woman is given all of the information on the medication used to manage the third stage of labour and she consents to this medication, it is her choice.
Recent research supports this very idea that “women should be given information on the benefits and harms of both [active and expectant management of labour] to support informed choice” (Begley et al., 2011).
Women’s views on active management versus expectant management of the third stage of labour
“The third stage was always something of a mystery to me. Physiological third stage was something always talked about by home birth women but not in hospital. On my first I never knew there was an option for the third stage. I had a spontaneous normal vaginal delivery and remember nothing about the placenta. I had the injection and it was out. No one even showed it to me. Unfortunately a small piece retained and I had quite a bad infection which affected breastfeeding. Despite this, I was sent home the day after I gave birth and ended up readmitted a few days later”
“On my second baby I was more informed and wanted a natural third stage and to leave the cord to finish pulsating. The hospital was never very upfront in the third stage and discussion was avoided. After the birth I was told I had irregular bleeding and placenta had to come out quick. I consented as I was worried. It was only after I got my notes that I saw I lost 400 ml of blood – and a PPH is defined as being over 500 ml”
“From my experiences, the hospitals treat the placenta and third stage as something to be feared, to be managed. I had all spontaneous normal births until the third stage, which was always managed quickly. Consent is implied and the injection is given. I only got to see my placenta if I asked”
“The hospital is so convincing that on my home birth I really felt apprehensive about a normal third stage of labour. I was worried about how long it would take and if it would be sore. It ended up being one of the best parts of my birth. I sat quietly in the pool feeding my new baby for an hour and a half just enjoying her still being attached to me. I started getting some gentle pains, we clamped the cord and I walked to bathroom as my midwife handed the baby to my husband. I sat on the toilet and my placenta came out with no effort. My midwife spent ages explaining the placenta and membranes to me. It was wonderful compared to my hospital births. It makes me realise that the fear around a normal third stage of labour is more to do with time management than what is best for me and my baby. Normal takes more time, so they insist on active management as best”
“On my third baby I was told I was not allowed to have a normal third stage as I had a previous PPH – they managed the third stage and cut the cord immediately. I was also sited with an IV just in case. it was only after getting my notes after the birth that I realised I never had a PPH on my previous birth!”
“When I gave birth to my first baby in hospital, I asked the midwife if I could wait and deliver the placenta without an injection. She agreed and gave me 45 minutes. When it came time to deliver the placenta, she asked me if I was ready and with a very gentle and easy push, the placenta emerged, completely intact. I didn’t know what to expect but I remember thinking: “that was easy!” and that it felt like a relief, after birthing my little baby”
Informed Consent and the Delivery of the Placenta
It is important to note that the drug Syntometrine® is contraindicated for breastfeeding infants. The Novartis information leaflet says this: “The use of Syntometrine during lactation is not generally recommended. Ergometrine is secreted into milk and the inhibitory effect of ergometrine on prolactin can cause a reduction in milk secretion. Syntometrine has the potential to cause serious adverse drug reactions in breastfed newborns/infants. Postpartum women receiving Syntometrine should avoid breastfeeding at least 12 hours after the administration. Milk secreted during this period should be discarded. Breast-feeding should be discontinued in cases where repeated postpartum administration of Syntometrine is necessary”. Please talk to your doctor or midwife about your birth preferences and ask that you are not given this medication if you want a physiological third stage and if you intend to breastfeed.
The HSE Clinical Practice Guidelines on Prevention and Management of Primary Postpartum Haemorrhage state that for “women without specific risk factors for PPH delivering vaginally, oxytocin (10 iu by intramuscular injection) is the agent of choice for prophylaxis in the third stage of labour.
Again, if a woman is low risk for postpartum haemorrhage (PPH) and would like to attempt a normal delivery of the placenta, this is not outside of the clinical practice guidelines and can be discussed with your doctor, midwife or other HCP. The recommended time to allow for the physiological delivery of the placenta ranges from 30 to 60 minutes after the baby is born, but it is not unusual for it to take a much shorter or longer time to emerge.
Encapsulating your placenta
Many women are now choosing to encapsulate their placenta. Whilst there are no RCT studies available at this time to draw definitive conclusions about the efficacy of this process, many clinical reports exist to indicate that placenta encapsulation is helpful in the postpartum period in terms of increasing milk supply (acting as a galactagogue) and improving mood in the postpartum period. There are various placenta encapsulators around the country, please make sure your encapsulator has sufficient training and experience in the process including certification in blood borne pathogens and also food handling and food safety. The Irish Placenta Association offer a list of practising encapsulators who have this basic training.
 AIMS Ireland
AIMS Ireland