Women’s experiences of Consent in the Irish Maternity Services
“What Matters to YOU?” 2014 Report on Consent in the Irish Maternity System.
The Association for Improvements in the Maternity Services in Ireland (AIMS Ireland) March 2014
1. Introduction
AIMS Ireland (Association for Improvements in the Maternity Services Ireland) is a voluntary organisation with charity status which was formed in 2007 by women who saw a need for a consumer driven organisation to support a woman’s human rights and her choices in childbirth, highlight healthy internationally recognised evidence based birth practices, and to provide support and information to women accessing maternity services in Ireland. It is a consumer led, campaign pressure group operating with a self-regulating committee elect and a body of members consisting of parents, consumers, health care professionals, and support group representatives throughout Ireland. AIMS Ireland was set up with the support of The Association for Improvements in the Maternity Services UK. AIMS UK has been at the forefront of improving maternity services the past 40 years.
In spring of 2014 AIMS Ireland ran an electronic survey on the topic of “What Matters to YOU?”. It was available through the AIMSI website (www.aimsireland.com), AIMS Ireland social media, parenting pages, and was also shared widely through social media channels (twitter and facebook groups), and Irishhealth.com
The second wave of results, a comprehensive look at care options and experiences, will be released on March 14, 2015 at the AIMS Ireland AGM.
2. Consent
This report looks at 2014 results relating to questions specific to consent, informed consent, and informed refusal in pregnancy, labour and birth, and during the postnatal period. These questions were designed to obtain current information on women’s experiences of consent in the maternity services. This is the second time AIMS Ireland has investigated consent, with a previous AIMS Ireland survey, “The availability of Information and Consent”, in which 161 respondents participated (2007).
AIMS Ireland were interested to re-examine the issue of consent, informed consent, and informed refusal in the 2014 survey with women whom have birthed in Ireland in the past 5 years to see if any notable changes have occurred in this area. We also hoped to reach a larger cohort of women.
3. Purpose and Design
AIMS Ireland sought to examine women’s experiences of consent between 2010-2014 in the following areas:
1) basic consent 2) informed consent 3) informed refusal
We define these categories as the following:
1) a broad statement of consent – was consent fully sought for all tests, procedures, treatments
2) informed consent – were benefits, risks, and potential outcomes fully explained for having/not having a test, procedures, treatment discussed
3) informed refusal – were women given the opportunity to decline a test, procedure, or treatment.
AIMS Ireland recognise that ‘informed consent’ and ‘informed refusal’ are both factors which generally define informed consent. However, for this survey the two were separated as:
1) Many women report to AIMS Ireland that they are supported in making an informed decision to have a procedure, test, or treatment, but they are not supported in declining tests, procedures, treatments – informed refusal.
2) The Irish National Consent Policy, citing the Irish Constitution (40.3.3), questions the rights of a pregnant woman to make an informed refusal; decline a medical procedure outside of recommendations by medical professionals.
AIMS Ireland asked respondents if consent was fully sought for all tests, procedures, and treatments in their pregnancy (ante-natal clinics, booking, etc), during their labour and baby’s birth, and during the post-natal period (following the birth of the baby). We also asked if women were provided with informed consent, provided with benefits, risks, potential outcomes for themselves and/or their baby to have or not have a test, procedure, treatment in pregnancy, labour/birth, postnatal period. And finally, if women had the opportunity to make an informed refusal.
The results are reported for ‘overall’ figures for the 2,836 respondents and then were broken down by care options in Ireland; Each of Ireland’s 19 obstetric led units, 1 private obstetric led unit (now closed), midwife led care options in Ireland, unassisted homebirth, and born before arrival (BBA).
4. Representation Frequency
There was significant representation of all the obstetric led units in Ireland and most other care options. However, some care options had limited responses which have implications on results.
Cavan MLU had only 2 respondents
unassisted birth had 9 respondents
born before arrival had 8 respondents
5. Quantitative Results: Pregnancy
Infograph #1 Overall basic consent in Pregnancy

Overall consent in pregnancy #WMTY2014
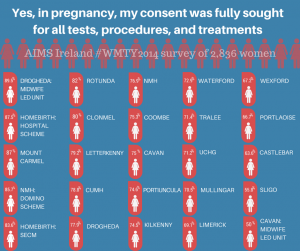
Infograph #2 Basic Consent Results in pregnancy by care option.
*note that for Cavan Midwife-Led Unit there were only two survey respondents.
________________________________________________
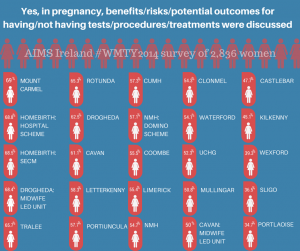
Infograph #3 Informed Consent in pregnancy results by care option.
*note that for Cavan Midwife-Led Unit there were only two survey respondents.
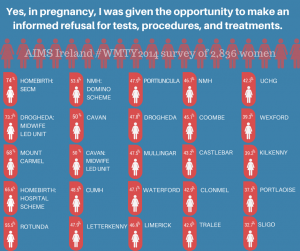
Infograph #4 Informed refusal in pregnancy results by care option.
*note that for Cavan Midwife-Led Unit there were only two survey respondents.
________________________________________________________________________________
6. Quantitative Results: Labour and Birth
Infograh #5 Overall Basic Consent Results in Labour and Birth
___________________________________________________________________________________
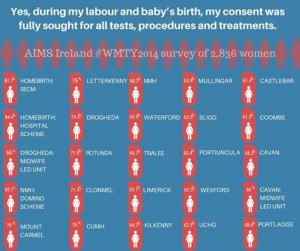
Infograph #6: Overall Basic Consent Results in Labour and Birth by care option
* note, Cavan MLU only had 2 respondents
___________________________________________________________________________________
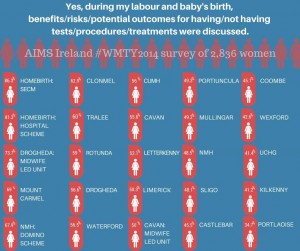
Infograph #7: Informed Consent in Labour and Birth by care option
* note, Cavan MLU only had 2 respondents
___________________________________________________________________________________
Infograph #8: Informed Refusal in Labour and Birth by care option
* note, Cavan MLU only had 2 respondents
________________________________________________________________________________
7. Quantitative Results: Postnatal Period
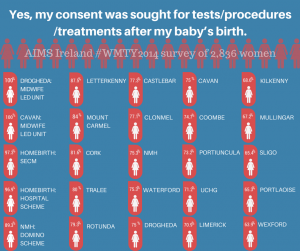
Infograph #9: Basic Consent in Postnatal Period (following birth of your baby)
________________________________________________________________________________
Infograph #10: Basic Consent in Postnatal Period (following birth of your baby) by care option
_______________________________________________________________________________
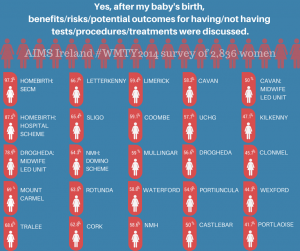
Infograph #11: Informed Consent in Postnatal Period (following birth of your baby) by care option
________________________________________________________________________________
Infograph #12: Informed Refusal in Postnatal Period (following birth of your baby) by care option
_______________________________________________________________________________
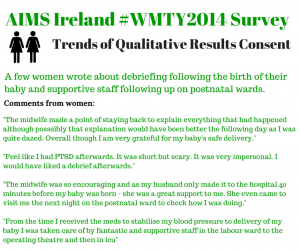
8. Trends in Qualitative Data.
The AIMS Ireland committee reviewed qualitative data for questions relating to consent and found that re-occuring trends appeared from the respondents who provided comments on the topic of consent. Basic consent issues, lack of choice regarding care options / routine tests, procedures, “not being listened to”, birthing described as “traumatic”, and feelings of having no control or choice were the most common phrases used by women in this section. There were comments highlighting positive care, “being listened to” and “having control” being the key phrases used by women who described their care as positive. Other women felt that consent was not relevant in their experience for a variety of reasons ranging from trust in medical professional’s recommendations, emergency situations, they felt no tests/procedures/treatments were initiated or suggested in their care, and the place or conditions of their birth (very fast, born without medical professional in attendance/born before arrival/homebirth).
Qualitative data mirrored quantitative statistics as many women felt that while consent was sought, suggesting an overall high rate for basic consent, they felt this was a ‘box ticking’ exercise and they did not really have a choice.
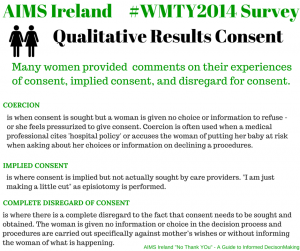
Three main areas were identified from women’s comments; coercion, implied consent, and a complete disregard for consent.
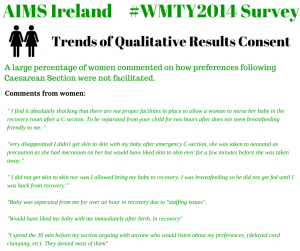
Infograph #13: Qualitative Results Consent
9. Comments from Women
Consent during pregnancy
1) Many women left comments with regards to the disregard for informed choice on care options / place of birth in Ireland; HSE exclusion criteria for Midwife Led Units (MLU), waterbirth, and homebirth.
“No, I refused CLU obs led care but was told too bad you can’t go to Mlu”
“I wish there was another box..I demanded the right to refuse a procedure. eg. I was not given the right to birth my baby at home with my Midwife, so I saw the hospital as a place to birth. I was not a patient, so refused to wear their ID bracelet.”
“Criteria for midwife led care are too strict. Because of my weight alone I was deemed ineligible”
“I was given no information on the MLU when I contacted hospital in Cavan to make my first appt.”
“I would have liked to have the option of waterbirth”
“I would have loved the option to give birth in a birthing pool. I don’t see why you have to leave the birthing pool for the actual birth.”
“As a non-Irish resident it is almost impossible to find out what choices there are outside of public hospital care.”
“I wanted a homebirth but was denied it on the grounds of a bmi over 30 and refusing a gtt”
“I was refused admission to the MLU in Drogheda based on a minor back condition yet I qualified for the HSE home birth. This makes no sense to me and I feel that more should be done to allow women to have a natural birth in places like the MLU and birth centres”
” I asked about homebirth on my first baby and GP told me it was unsafe and unavailable to me which wasn’t true”
“Women should have the option to hire a private midwife in a public hospital and not just a private obstetrician in a public hospital as is currently the case”
2) A few women commented on how they felt pressured into tests, procedures, treatments (particularly GTT) in pregnancy in order to avail of their choice of care option.
“At my booking appointment, where I told the consultant I was opting for a homebirth with a SECM I was bullied into agreeing to GTTs and growth scans. Neither of these were clinically indicated. While I felt the only option open to me was to agree with the consultant, I very promptly cancelled them”
3) Many women commented on a lack of information to assist them to make an informed decison / informed refusal.
“Felt that sweeps and interventions to bring on labour were being offered very freely without explaining what they were or what might happen.”
“I felt angry at my full term appointment when i said I didn’t want to discuss induction until I was at least 14 days “over”. When i said I didn’t want a sweep on that day I was asked if I knew the risks involved in not intervening (stillbirth being one). Risks like infections from unnecessary sweeps weren’t mentioned.”
“Midwives and junior doctors I met were reluctant to engage in discussion about reasons for and pros/cons of tests for diabetes and scheduling induction. Just parroted the hospital policy at me, without giving me extra info or being open to addressing my concerns.”
“Everything was always rushed and barely explained, there was always a sense of the midwives being too busy and that you were only annoying them by asking questions.”
4) Women commented that in pregnancy there was a perception of assumed consent from care providers with routine tests/procedures/treatments in accessing ante-ntal care.
“I was just told these tests are standard everyone has them. I actually had to follow up myself on the results from blood tests to see what the results had been.”
“In the hospital and with the doctor unless I refused the procedure it was assumed that I would go ahead with it. I was told that it was happening, not asked if I wanted it to happen.
“The tests they did were as far as I was told compulsory and results were just told to me and options were not discussed it was there way is best. When we questioned it we were told we were putting our babies life in danger.”
“I felt that I could not say no to anything. You have to put all of your trust in the medical professionals. Sometimes they are wrong.”
“I refused plenty, but they weren’t put as questions. Statements like “we’re just going to” or “ok, so now we’ll” had to be responded to quickly with a NO, you won’t, and that wasn’t always “heard”.”
5) Several women commented that they did not understand why recommendations would be declined.
“Tests suggested or recommended were for my or my baby’s benefited – it would never have occurred to me to refuse. Why would I?”
6) Many women left comments describing expressions of guilt or being lied to regarding informed consent / informed refusal in pregnancy.
“You were made to feel a bad mother if you did not have all the tests.”
“I didn’t feel that I needed to be tested for gestational diabetes and was made to feel bad for not getting the test when it was recommended. The test was negative but the procedure loeft me sick for a few days afterwards”
“Not without being made feel very guilty.”
“i was strongly encouraged not to refuse!”
“I felt I was lied to”
“I had to challenge the hospital on everything. Procedures and “policy” were proposed that were against HSE best practice, best practice in UK, US and most of Europe and that have been proven to have NO benefit to mother or baby and only bring increased risks.”
7) Women commented on how the format of the Irish maternity system, or logistics (under-staffing) affected informed consent / informed refusal.
“there were always too many mothers to have quality time with any of the professionals in the hospital..”
Hospital visits were always different … Different consultant , different information… So I never felt fully informed anyway
8) Women commented with examples of feeling ‘bullied’ into consent for tests/procedures/treatments in pregnancy or provided examples of disregard of consent.
“I was instructed that I wouldn’t have the option to refuse monitoring during labour. I wanted the option to refuse monitoring (FHM) during labour to move around and be more mobile if I desired.”
“I had an amnio because of pressure from obs who did not fully explain risks and then let a reg do the procedure.”
“When a sweep was suggested at 39 weeks. I refused and then was convinced by doctor to let her dp the sweep. Looking back I felt bullied and as I was tired I caved and consented to it”
“Due to being .4 over the “limit” for BMI and being classified as obese, I was informed I had to take the GTT, even though I had no other risk factors. I was not informed that it was within my rights to refuse. If I had weighed just 1kg less, I would not have had to do it, especially annoying that I was asked to drink as much as possible that morning for the ultrasound. Without that I would probably have been under the limit.”
“I gave informed refusal for VEs, pethadine and managed 3rd stage but the midwives did not agree with my choices and I had to repeat numerous times and felt bullied. I very firmly said I didn’t want pethadine or syntometrine they prepared both of these anyway and had them sitting ready!”
With the Swine Flu / Flu injections being specifically cited in many instances:
“I still feel i was bullied into swine flu vaccination against my better judgement in during my third pregnancy in 2010.”
“Only problem I had was a doctor trying to force me to have the swine flu jab he was very aggressive towards me otherwise all other medical staff where great”
9) Women commented on self-advocacy and provided examples in which they were supported in informed consent / informed refusal in pregnancy; though sometimes describing this as a ‘fight’ for some women in some instances.
“I wasn’t given the opportunity, but I took it because no-one touches me without my consent. I’m one of the hundreds of thousands of women who has survived sexual assault, consent is a massive deal for me. As it should be for every single healthcare practitioner.”
“With the caveat that you have to be self-informed also. The hospital were running a study which involved continuous monitoring: half the subject were to receive continuous monitoring during labour and the other half would not receive continuous monitoring. I knew that I did not want continuous monitoring and did not want the risk of being randomly assigned to the study group, so declined to sign the permission form. This was fine.”
“If you refuse things in (hospital named) then my experience is that they take a dim view of this and treat you accordingly. My own consultant has only ever been the only medical professional who respects my own mind, ironically enough.”
“I had to fight tooth and nail not to be induced at 6 days over.. no medical reason to be induced. Just to suit induction days in hospital. Only that I was relatively self informed that I refused but it was not made easy for me”
“Eventually…. GTT refused but not without a fight.”
“Not really. I did refuse and they got very cross. I got my way but only as I was very, very vocal and prepared to walk away from the scheme.”
Consent during labour and birth
Trend #1: Many women responded that while consent was sought, they often felt they did not have a choice.
“Consent was sought at all times but I felt pressure that the only option was to agree with what was proposed.”
“Formally yes (consent was obtained), but I wasn’t in favour of being induced, it was never presented as an option but rather as a decision made on my behalf.”
“most things were not presented as a choice. “We have to do such and such” was the usual “choice.”
” I repeatedly impressed my wish not to have oxytocin and this was disregarded and I was treated like I was being silly. I reluctantly agreed but I felt badgered into submission rather than consenting.”
Trend #2: AIMS Ireland also found that many women were cited with ‘hospital policy’ and/or risk to their baby in order to obtain consent.
“Benefits of procedures to hurry Labour up were told, risks of these procedures were not told. Benefits of waiting were never once told.”
“Requested c-section based on 2 previous traumatic births (incl 1 section) but was bullied into natural birth – best for baby.”
” I didn’t want to be induced but in (unit named) the policy was to induce when 10 days over; I didn’t agree with this policy but felt I had no choice but to comply”
” I found the midwives wanted me on my back for birthing as it was easier for them and that even when I requested to kneel as I had no power to push that this was not supported”
“At every intervention I was threatened with catastrophic consequences if I refused such as ‘if you don’t have an episiotomy right now the baby won’t make it’…’if you don’t take antibiotics the baby might have cerebral palsy’”
“I was told by the midwife that I had to have my waters broken in order to get an epidural (I found out afterwards this is actually not hospital policy).”
“I was told I had no choice when it came to my treatment, everything was ‘hospital policy’”
“My consent was sought but I was very much led to believe it would be negligent not to consent”
“nothing was done without my ‘consent’, but is it consent when you are bullied into it… as how do you get round the ‘put the baby at risk’ card even if you know that what you are asking is in line with best practice…?”
Trend #3: Other women described how procedures were performed without consent with many women citing breaking of waters, episiotomy, membrane sweeps, and foetal scalp monitoring/CTG as issues:
“Did not know my waters were going to be broke at examination the doc just did it thought she was just checking how the gel was working.”
“A fetal scalp electeode was applied to my baby and an arm was performed without seeking consent. The only reason I was told the fse had been applied was because I noticed the different sound of the fhr beat on the ctg”
“They broke my waters without consent. I was told by the consultant that she did not need my permission to break my waters.”
“The following procedures were performed on me without explanation or my consent being sought: – ARM – Pushing back a cervical lip A CTG machine was applied to me and when I asked for it to be removed this was refused. My attempts to remove it myself were prevented. I was also physically restrained in a position I was not comfortable in (flat on my back) and verbally abused when I did not want to engage in purple pushing.”
“My consent was only sought for internal exams. I was given an episiotomy without being asked. I wasnt even informed that the consultant was going to do one it was just done. I was given drug to deliver placenta without my consent or knowledge even though I had on my birth plan that I did not want either an episiotomy or injection for placenta delivery”
“Monitor placed on baby’s head without telling me what they were doing”
Trend #4: Many women described their experience very emotively
“It was awful, felt like medical rape.”
“I found it very traumatising and felt that no one listened”
“No permission sought for anything. Intervention for no reason. Treated like a lump of meat.”
“Never setting foot in (hospital named) again”
Trend #5: Others described very supportive care where care providers went out of their way to ensure that women were informed and decisions were supported.
“very thorough info given before c section and it was repeated on several occasions”
“The midwife assigned to me was very very empowering as she saw my hopes for a natural birth disappear… she made me feel that I was in control throughout the labour and was very conscious of my need to be guided rather than forced into anything. At times the supervising nurse was suggesting moving things along and my midwife was very firm in her support for me, my partner and our rights. This means that despite a somewhat traumatic birth experience I didn’t feel ‘voiceless’.”
“Even though I was induced, had waters broken, put on a drip (all due to previous stillbirth) I made all of those decisions, decided when they would do things, how they did them. They listened carefully to me, and I was in total control of my birth”
Trend #6: Other women felt that consent was not applicable to them, did not arise, or that they trusted health care providers in their recommendations.
“8cm when arrived in hospital”
“My birth was very fast so there wasn’t time for tests, etc. Midwife did explain everything she did though”
“At one stage I was barely conscious so consent was obtained from my husband”
“I had an unassisted birth”
” I was absolutely out of my mind on pain relief and I can’t even remembering them asking”
” Crash section, no time”
“Not enough time, had to trust my midwife completely”
” Homebirth with a SECM”
Trend #7: Others were able to make an informed decision but described this as being difficult ‘a fight’ or being down to experience.
“I had to fight hard, and I still didn’t get the birth I wanted. I got the birth I wanted in the sense that my baby and I are well and I didn’t have interventions, but it wasn’t pleasant in the hospital.”
” I felt I had to be very vocal/pushy to have my concerns listened to”
” I was listened to because it was my second baby and I forced people to listen to me – you learn from the 1st experience”
Comments from women: consent following the birth of their baby
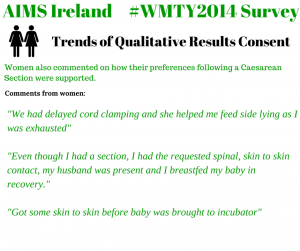
1) There was a very large response from women who commented on how their preferences following Caesarean Section were not facilitated.
2) Some women commented on how their preferences following a Caesarean Section were supported.
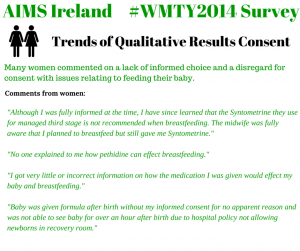
3) Many women commented on a lack of informed choice and a disregard for consent with issues relating to feeding their baby.
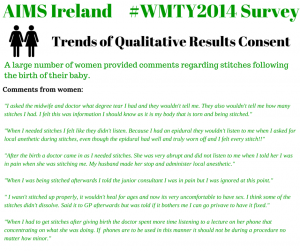
4) A large number of women provided comments regarding stitches following the birth of their baby. Trigger warning, some comments may be distressing for some readers.
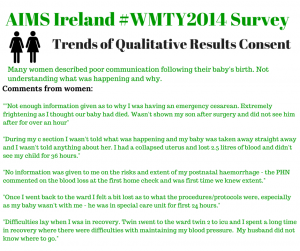
5) Many women described poor communication following the birth of their baby. Not understanding what was happening or why.
6) A few women wrote about debriefing following the birth of their baby and supportive staff following up on postnatal wards.
Numerous women discussed busy and understaffed labour, birth, and postnatal wards which affected their care.
” Midwives minding 2 labouring women at once while covering each other’s breaks – I did not expect this and it panicked me a bit”
” Hospital was extremely busy. While I like being left alone in labour this was ridiculous”
” There was simply not enough experienced midwives on duty the night I had my baby. I believe I would have had a very different and more positive experience if there had been.”
” No beds available. Left to labour alone w/partner on corridor in admissions. No privacy. No monitoring. No pain relief.”
” I had the sense that staff simply did not have the time to take into account the wishes/aspirations of mothers. I think they would have liked to be more welcoming and to have listened more but did not have the opportunity.”
” The unit is understaffed and out of date by at least 20 years. Breastfeeding is discouraged.”
” I felt that everyone was doing their job and did look after me to the best of their ability however the induction room was full and there were not enough staff. There were times I was left in unnecessary pain.”
“I asked for an epidural at 3pm and only received it at 11pm because there was no staff to look after my in the labour room. Had to wait in the pre-labour ward and was told that it was OK to give birth there, other people had done it!”
“The professionalism and knowledge of midwife taking care of me was second to none but she was very busy when I was at the pushing stage, attending to two other women at the same time who were also at the pushing stage”
“Staffing was very limited but the midwives were amazing in still keeping up a level of care that I was happy with although I could see that they were being pulled from one place to another especially on the post natal wards. 3 midwives at night and one of those a student, for 33 patients on the ward.”
“Husband was given alarm button during birth as only one midwife available for delivery”
“can be a very scary time for a first time mother staff are very busy and at times can be snappy and not listen to you. when I was in the pre labour ward I knew I needed to go to the labour suite the midwives did not listen to me and then when they did check I had to be rushed up. once my baby was born I was wheeled into a corridor and the midwife opened my top to breast feed infront of other dads waiting there who could visabily see both breasts! following this I was moved to the public ward despite being a semi private patient and wedged between two other beds with no light and left there in the dark holding my baby. I did not have a bell to get assistance when I became ill an hr later and had to ask one of the other women who had also given birth to get assistance”
“Junior doctors on strike day I was brought in for induction”
“Due to midwife shortages my induction was started then stopped until the next shift came in.”
10. Conclusions
The findings of nearly 3,000 women, whom had given birth in Ireland in the past 5 years (2010-2014), found that while 67% of women agreed that basic consent had been sought during labour and birth, 52% of those surveyed did not receive information on potential implications to have or not have tests, procedures, treatments to assist with their decisions, and only 50% felt able to make an informed refusal during their labour and baby’s birth. These trends were mirrored in results in pregnancy and during the postnatal period.
Further, results of consent practices in the various care options available in Ireland suggest that care models (medical/obsetric vs physiological/midwife led), ‘where’ and ‘with whom’ a woman accesses maternity care had an influence on her likelihood of informed decision making. With rates ranging from 86.3% to 34.7% for informed consent in labour and birth and 89% to 31.4% for rates of informed refusal during labour and birth.
While the overall rates for basic consent appear high, the quantitative statistics suggest that informed consent and refusal remain an issue of concern with only 50% of women being provided with the necessary information to assist them in informed decision making. The qualitative data, comments from women, provide us with very worrying information as many women commented that consent was either implied as the procedure was being carried out “we are just going to break your waters now” as rupture of membranes was being performed, coerced by hospital policy or perceived risk to baby, influenced by care providers opinion not based on evidence, were not provided with information necessary to make decisions for themselves and their baby, or women felt that while they consented, they did not have any choice in doing so.
Positive comments from women showed that a supportive care provider is very important in women’s overall experiences and likelihood of informed decision making. In instances where complications arose and it was medically necessary for the woman’s care to deviate from her preferences, being informed and included in decision making and being “listened to” gave women a sense of control and a more positive experience.
The survey also showed that consent and informed consent/refusal were higher for procedures, tests, treatments in pregnancy and the postpartum period (following the birth of the baby) than during the labour and birth, which AIMS Ireland contribute to underlying issues in Ireland’s National Consent Policy.
The Irish National Consent Policy directly questions a pregnant woman’s right to refuse treatment. This has a serious implication on a woman’s right to make informed decisions outside of clinical recommendation in Ireland. The drop in rates of consent and informed consent/refusal during the time of labour and birth suggests that this policy is very much reflected in practice within Irish maternity units.
Many women commented on staff shortages of midwives to look after them in labour, birth, and following the birth of their baby; providing examples of the implications of shortages on their experience and care. AIMS Ireland have raised the issue of midwife : woman ratios in Ireland previously, with many units falling far outside recommendations.
11. Recommendations
AIMSI would recommend that the issue of consent and provision of unbiased, complete information become areas of importance with Irish maternity units. “Hospital Policy” should not over-ride or give illusion of consent and individual choice for care options, admission, and opting in or out of procedures, tests and treatments. Consent policies should be revisited and printed material become available for every woman booking into maternity units.
Women should be informed of all the benefits, risks, and potential implications for themselves and their baby to have or not have procedures, tests, treatments, and interventions in order to make the best decisions in their circumstances. Women cannot truly give consent unless they understand what it is they are consenting to and are supported in these decisions by health care providers.
AIMS Ireland recommend strongly that a National clinical guideline is implemented to support the principals of informed decision making in Irish maternity services. To facilitate guidance of this, obstetric units should be under obligation to implement already existing National clinical guidelines for evidence based care rather than routine policy which relies heavily on medical management.
Further, HSE must come in line with best practice Midwife : Woman ratios of 1:28 for low risk case loads and 1:25 for high risk case loads to ensure supportive and safe care for women and their babies. Current Midwife : Woman ratios in Ireland range from 1:30 to 1:55.
Further Reading:
Midwife : Woman ratio levels per obstetric unit here: http://nocountryforpregnantwomen.blogspot.ie/2014/03/revealed-midwifery-staffing-levels-for.html
Return to Results of What Matters to You 2014
 AIMS Ireland
AIMS Ireland